Nausea and Perimenopause: A Complete Guide
Have you been feeling a bit queasy lately?
Is your nausea becoming too common to write off as a weird thing you ate?
Most of us know, or maybe have even experienced the nausea that can come with pregnancy. Some of us may even get nauseous at certain times of our cycle.
But could this new nausea you’re experiencing be a symptom of perimenopause?
We know that around 90% of women experience at least some menopausal symptoms in their lifetime.(1)
Even though we don’t know the exact numbers of women who suffer from nausea during perimenopause, we do know it is a common problem that a lot of women are talking about. In fact, 50% of my Instagram followers answered ‘yes’ to experiencing nausea with their perimenopause on a recent poll.
So, you are definitely not alone.
This easy-to-understand guide will walk you through the basics of why your nausea may be happening, what to do about it and when it’s time to seek professional help.
Let’s get going.
What Is Perimenopause?
Perimenopause consists of the symptomatic period “around the menopause” (2). In general, it begins with changes in the menstrual cycle and ends around one year after your last period.
The time refers to the hormonal, body and psychological changes that can happen during this time of transition.
What are the symptoms of perimenopause?
Perimenopause can come with a whole host of symptoms, so what else could be pointing you towards perimenopause as a reason for your new-found nausea?
Common perimenopause symptoms are:
Hot flashes and night sweats
Vaginal dryness
Altered mood and sleep
Heart palpitations
Hair loss
Weight gain
Changing menstrual cycles
Foggy brain and forgetfulness (3)
Irritation and mood swings
Even though there is not a lot of research done on digestive symptoms related to perimenopause, some common symptoms include:
Constipation
Diarrhea
Acid reflux and heartburn
Abdominal pain
Bloating (4)
Note: these are also menopause symptoms - it’s just that menopause can only be diagnosed 12 months after your last period.
What Does Nausea Have To Do With Perimenopause?
There isn’t a ton of research on nausea and perimenopause specifically, but experts know it does happen to some women and they’ve got some well-formed ideas as to why.
Hormones such as estrogen and progesterone rise and fall in our ‘transition’ periods such as pregnancy and perimenopause, but for our purposes today let’s focus on estrogen.
Most of us know that estrogen plays an important role in a women’s reproductive system but what you may not know is that it is involved in many other areas of our health (5).
Estrogen plays a role in our bone health, immune system, vascular health (the network of blood and other vessels) as well as our gut.
When our estrogen levels fluctuate, our bodies mostly adjust to this change but the gut, and how it functions, is affected (6,7).
These hormonal changes, particularly with estrogen, can cause digestive complaints, including the nausea you’re experiencing. This is also why we can also experience diarrhoea and bloating during certain times in our menstrual cycle and pregnancy (8).
This is also why if you are taking estrogen as HRT ( hormone replacement therapy ), nausea can be a side effect.
If your nausea becomes unmanageable, do discuss with your doctor/GP about changing the route (tablets, patches, implants, rings, creams, etc.) reducing the dose or type of your HRT (9).
Help Ease Your Symptoms Of Nausea
There are several ways to ease your perimenopausal nausea, in this article we’re going to focus on practical nutrition and lifestyle tweaks.
Knowing the reason why you’re experiencing nausea is really important. Nausea can be caused by fluctuating hormones and/or HRT but there may be something else going on entirely.
Always speak to your doctor/GP so they’re aware and can provide the appropriate care.
Our tips to try for relieving nausea:
*BONUS: they may help other symptoms too*
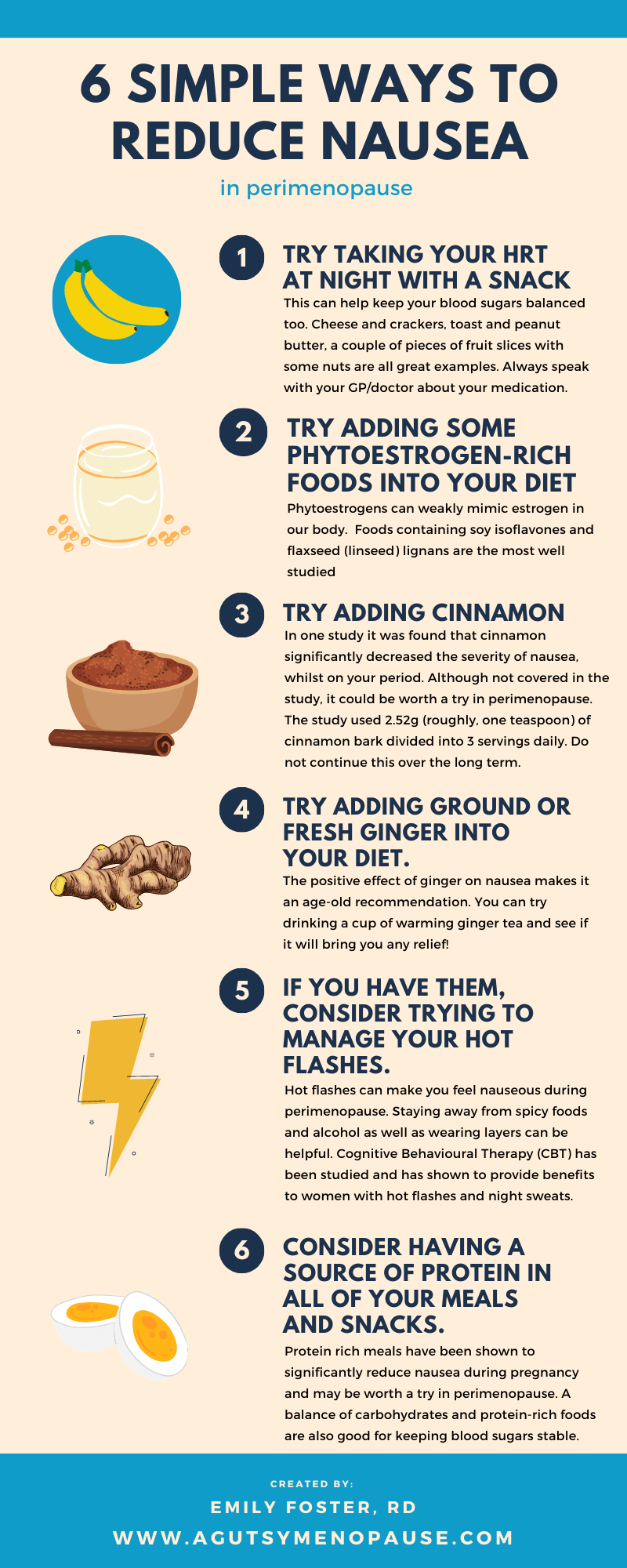
Try taking your HRT at night with a well-balanced snack:
This can help keep your blood sugars balanced too. Cheese and crackers, toast and peanut butter, a couple pieces of fruit with some nuts are all great examples. If this doesn’t help, discuss changing to another type of HRT with your doctor (10).
Try adding some phytoestrogen-rich foods into your diet:
This is not likely to make a life-changing difference but if your nausea symptoms are mild it may be worth a try. Phytoestrogens can weakly mimic estrogen in our body.
Foods containing soy isoflavones and flaxseed (linseed) lignans are the most well studied (11) foods containing phytoestrogens. You can take these as a supplement or try to eat foods containing soy and/or flaxseed (linseed). (12)
Try adding cinnamon to your drinks or food:
In a 2015 study, it was found that cinnamon significantly decreased the severity of nausea, among other symptoms, whilst on your period. Although not covered in the study, it could be worth a try in perimenopause. (13) The study used 2.52g (roughly, one teaspoon) of cinnamon bark divided into 3 servings daily. Do not continue this over the long term.
Try adding ground or fresh ginger into your diet.
The positive effect of ginger on nausea (14) makes it an age-old recommendation. You can try drinking a cup of warming ginger tea and see if it will bring you any relief!
Other Ideas with ginger:
Ginger iced tea: Sliced ginger, lemon and spoonful of honey - make warm, let steep for 15 minutes, then place in the fridge for an hour (or overnight, ready for the next morning). Serve with ice.
Ginger chews/sweets: We don’t want to have too many of these as there can be quite a high amount of free (added) sugars but a couple of these may do the trick. you can choose a sweetener-based sweet if watching your blood sugars. Beware that if there is a sugar alcohol (ending in ‘ol’) sweetening the product this may cause gut distress for those with GI symptoms and/or IBS.
Try having a recipe featuring ginger for dinner: We found this great ginger chicken recipe from BBC Good Food.
If you have them, consider trying to manage your hot flashes.
Hot flashes can make you feel nauseous during perimenopause. Staying away from spicy foods and alcohol as well as wearing layers can be helpful. Cognitive Behavioural Therapy (CBT) has been studied and has shown to provide benefits to women with hot flashes and night sweats (15).
Consider signing up for a programme or purchasing a self-help workbook, the workbook “Managing Hot Flushes and Night Sweats: A Cognitive Behavioural Self-Help Guide To The Menopause”* by Myra Hunter and Melanie Smith. This workbook was shown to be as effective as eight hours of CBT in a recent study.
*Disclosure: We have an affiliate relationship with books purchased through our affiliate link at Bookshop.org (these guys are pretty cool - they support independent book shops). In a nutshell, everytime you buy a book with our link, we earn a small commission. Thanks!
Eat smaller portions more often.
Experiment and see what works for you but smaller portions may be easier on your stomach and reduce the severity of your nausea (16).
Cooler foods and drinks.
You may find cold food and/or drinks can be better ‘stomached’ when you’re feeling nauseous. The reduced smell of the food and/or drinks can make it easier.
Consider having a source of protein in all of your meals and snacks.
Protein rich meals have been shown to significantly reduce nausea during pregnancy and may be worth a try in perimenopause (17). A balance of carbohydrates and protein-rich foods are also good for keeping blood sugars stable.
Protein rich foods include:
fish (e.g. salmon, cod, tuna)
cottage cheese
yoghurt & milk (dairy & soy options only - dairy alternatives such as oat, rice and almond very rarely have protein)
beans & lentils
nuts & seeds (almonds, chia seeds, pumpkin seeds)
soy products (e.g. tempeh, tofu, edamame)
‘Sister-Symptoms’ That Can Accompany Nausea
When we say ‘sister-symptoms’, we mean symptoms that can often accompany your nausea, and point towards perimenopause.
Dizziness: Feeling dizzy can be a symptom of many conditions but it is associated with perimenopause too. Hormones are one to blame for this. The fluctuation of estrogen and progesterone can cause dizziness (18).
Bloating: Decreased or low ovarian hormone levels might have the reason for your bloating. If your bloating and pain last 3 or more days, speak with your doctor/GP (19).
Headaches: Headaches, especially migraines, are related to ovarian hormones. During times of changing estrogen, such as in perimenopause, headaches can be temporarily worse (20).
Constipation: Women who are in perimenopause are more prone to have constipation than women who are not (21).
When To See A Medical Professional?
If nausea is affecting your daily routine and/or feels unmanageable, it is best to speak to your doctor/GP.
Nausea is also related to a bunch of other health conditions.
Finding the reason for your nausea with a healthcare professional can be helpful as well as important.
Remember to mention any episodes of vomiting or diarrhoea in addition to any accompanying ‘sister-symptoms’ to your doctor/GP for diagnosis and treatment.
In Summary
We know that around 90% of women experience at least some menopausal symptoms in their lifetime.
One of the many symptoms can be nausea.
There isn’t a ton of research on nausea and perimenopause specifically, but experts know it does happen to some women and is most likely related to fluctuating hormones, particularly estrogen.
There are many ways to help ease symptoms of nausea in perimenopause, some of these include: having protein-rich meals and snacks, taking HRT at night time with a balanced snack and trying to manage your hot flushes with CBT.
Remember that nausea is also related to a bunch of other health conditions. Consult with your doctor/GP if it is affecting your daily life and/or if your symptoms worsen.
Want to save this article? Click here to get a PDF copy delivered to your inbox.
A Gutsy Menopause is a specialist gut health nutrition clinic run by nutritionist and dietitian, Emily Foster. We offer consultations, workshops and online courses.